An international collaboration led by scientists from the University of Cambridge and Berlin Institute of Health at Charité (BIH) has discovered more than 300 regions in the genome that contribute to each person’s individual chemical fingerprint. Their results, published today in Nature Medicine, show how variations between individuals at these regions affect how our body reacts to external influences, which diseases we are susceptible to and how severe an illness will be.
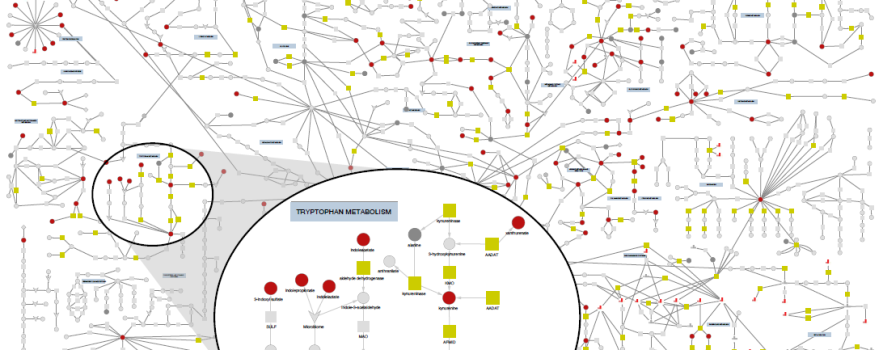
Our body continuously processes thousands of small molecules such as fats, proteins and sugars as part of our normal metabolism, and the levels of these metabolites vary from person to person. Small changes in this individual chemical fingerprint can cause or reflect illness, and potentially provide useful information about a person’s health. The scientists discovered both rare and common changes in the genetic code that influence this personal chemical fingerprint and an individual’s disease profile. ”
Professor Claudia Langenberg, Professor at the Berlin Institute of Health, and was an MRC investigator and programme leader at the MRC Epidemiology Unit when this work was done commented:
With our study, we are finally illuminating the genetic control of our metabolism based on many hundreds of small metabolites, which has never been shown in such detail. This means we now better understand how and why genetic differences contribute to the development of diseases.”
The scientists measured the amount of more than 900 small molecules in blood samples from over 14,000 participants in two large UK population studies – the INTERVAL study and the EPIC-Norfolk study – whose genetic code had also been analysed. They identified 330 regions in the genome that are linked to the levels of 646 different metabolites, with most regions linked to several metabolites, and vice versa.
Professor Langenberg said.
These metabolic ‘hotspots’ in the genome have helped us to better understand which genes are relevant to the changing amounts of molecules in the blood, with these new findings, we were then able to show which changes in metabolism contribute to the development of individual diseases, such as breast cancer”
Among the examples of the influence of metabolites on disease that they identified was an association between an increased levels of the modified amino-acid homoarginine and an increased risk of chronic renal failure. Homoarginine is currently in clinical trials for the prevention of cardiovascular disease, so special attention should therefore be paid to monitoring and maintaining kidney function in trial participants.
In addition to a role in healthy metabolism or disease, the scientists identified variations in the metabolic ‘hotspots’ in the genome that affect how effective drugs are, and the severity of their harmful effects. For example, the scientists found that about one fifth of the study participants had variations in the genetic code close to the DPYD gene. DPYD encodes for an enzyme that is responsible for breaking down certain common cancer chemotherapy drugs, and people these genetic variants are at an increased risk of accumulating elevated levels of these drugs and consequently more severe effects.
Professor Langenberg commented.
Variations near genes that are also the target of drugs can give us clues about possible unwanted side effects. For example, we were able to show that drugs that reduce the conversion of steroid hormones in the body and thus counteract male hair loss and prostate enlargement may increase the risk of depression, which is consistent with reports from drug studies”
The paper is the result of many years of cooperation between scientists at the University of Cambridge and BIH, as well as colleagues from all over the world including the Helmholtz Centre in Munich, Weill Cornell Medicine – Qatar, Pfizer, and Health Data Research UK. The team has made the summary statistics from their work publicly available to the scientific community through the interactive webserver omicscience.org, and the metabolite raw relative abundances for this paper are available in the MetaboLights database.
Information about an individual’s chemical fingerprint and the genomic variations that underpin it could help clinicians to more effectively tailor treatments to individual patients, and Professor Langenberg is already leading a new initiative to support this, saying:
We need larger studies that better map the genetic diversity of different populations to understand the biological and clinical effect of genetic variations that differ between certain populations.”
Read more
- Praveen Surendran, Isobel D. Stewart, Victoria P. W. Au Yeung, Maik Pietzner et al. Rare and common genetic determinants of metabolic individuality and their effects on human health. Nature Medicine 10 November 2022. DOI: 10.1038/s41591-022-02046-0

 MRC Epidemiology Unit
MRC Epidemiology Unit